2. 中国农业科学院与世界农用林业中心农用林业与可持续畜牧业联合实验室, 北京 100193
2. Chinese Academy of Agricultural Sciences and World Agroforestry Center Joint Lab on Agroforestry and Sustainable Animal Husbandry, Beijing 100193, China
腹泻是新生犊牛常见的肠道疾病,可降低其成年后的生产性能[1-2],多发生于出生3周龄以内[3]。引起犊牛肠道感染的主要病原体包括大肠杆菌K99、轮状病毒、冠状病毒、沙门氏菌和小隐孢子虫等[4-5]。大肠杆菌和沙门氏菌感染引起犊牛腹泻后往往用抗生素进行治疗,但因为不当使用抗生素会导致严重的抗生素耐药性问题[6]。因此,为了减少抗生素在食物链和环境中的存在,寻找促进动物机体健康生长且安全环保无残留的饲料添加剂成为目前饲料领域的研究重点,其中植物及其提取物[7]、多酚类物质[8-9]、微藻[10]和微生态制剂[11-12]等已广泛用于动物饲养中。
裂壶藻(Schizochytrium sp.)是一种可以通过发酵培养的微藻,其不仅富含n-3多不饱和脂肪酸(n-3 polyunsaturated fatty acids,n-3 PUFAs),而且也含有酚类化合物等具有抗氧化作用的物质[13]。n-3 PUFAs可调节免疫功能且具有抗炎和抗氧化等生理功能,并能够促进动物生长发育[14-19]。裂壶藻作为新型饲料资源,对水产动物、家禽和猪的生长和免疫等均有积极促进作用[20-22],然而在犊牛上的应用研究较少。
乳铁蛋白(lactoferrin)具有广谱抗菌性[23-24],对大肠杆菌的抗菌作用尤为显著[23, 25-26]。此外,乳铁蛋白还可调节机体免疫[27],提高抗氧化能力[28],并保护肠道屏障功能[29]。目前认为乳铁蛋白对新生动物胃肠道发育的益生作用主要是通过抑制细菌生长[30]、促进肠道细胞生长[31]、促进肠道葡萄糖吸收等[32]。乳铁蛋白的抑菌作用可保护新生犊牛的肠道不受感染,促进肠道细胞的生长,增加肠道对免疫球蛋白G(IgG)和营养物质的吸收[33]。然而,乳铁蛋白在犊牛上应用的研究结果并不一致。Robblee等[34]通过在断奶前犊牛饲粮中添加0、1、2和3 g/d乳铁蛋白对生长性能及粪便评分进行研究,结果表明,饲粮中添加1 g/d乳铁蛋白可降低断奶前犊牛粪便评分以及腹泻治疗天数;但Joslin等[33]在断奶前犊牛饲粮中添加0、1和10 g/d乳铁蛋白的研究发现,饲粮中添加1 g/d乳铁蛋白对粪便评分没有显著影响。Yekta等[35]研究了乳铁蛋白对绵羊大肠杆菌O157:H7攻毒后肠道中的定植和排泄规律,结果表明,乳铁蛋白可以减少粪便中大肠杆菌O157:H7的排出量和持续时间。然而,Kieckens等[36]研究发现,口服乳铁蛋白并未有效降低犊牛粪便中大肠杆菌O157:H7含量,但乳铁蛋白经直肠给药可有效降低粪便中大肠杆菌O157:H7含量。
目前,关于裂壶藻在哺乳犊牛中应用很少,且裂壶藻和乳铁蛋白是否存在协同效应并无相关报道。因此,本试验通过对大肠杆菌K99攻毒处理的哺乳犊牛饲喂裂壶藻和乳铁蛋白,研究裂壶藻和乳铁蛋白及其协同效应对犊牛腹泻的缓解作用,以及其对腹泻犊牛生长性能和抗氧化能力的影响。
1 材料与方法 1.1 试验材料裂壶藻:干物质(DM)含量为97.69%,粗蛋白质(CP)含量为13.76%,总脂肪含量为46.80%,二十二碳六烯酸(docosahexaenoic acid,DHA)含量为每100 g脂肪23.65 g;乳铁蛋白纯度为95%;大肠杆菌K99购自中国兽医药品监察所,菌株号为CVCC 237,血清型为O101:K99。
1.2 试验设计与饲养管理本试验在山东省东营市东营澳亚牧场进行。选取50头1日龄新生荷斯坦公犊牛,随机分为5组,每组10头牛。对照组(C组)饲喂基础饲粮,不添加乳铁蛋白和裂壶藻;乳铁蛋白组(LF组)饲喂基础饲粮+1 g/d乳铁蛋白;裂壶藻组(SZ组)饲喂基础饲粮+20 g/d裂壶藻;乳铁蛋白+裂壶藻组(LF+SZ组)饲喂基础饲粮+1 g/d乳铁蛋白+20 g/d裂壶藻。同时设置未攻毒大肠杆菌组(non-challenged E. coli group)进行参考比较。乳铁蛋白添加量参考Robblee等[34]研究结果,裂壶藻添加量参考预试验结果。乳铁蛋白和裂壶藻从犊牛2日龄开始混合在牛奶中进行饲喂。在7日龄时,除未攻毒大肠杆菌组外,对其他各组试验犊牛进行大肠杆菌K99攻毒,攻毒方式为于晨饲前将1 g含量为1×1011 CFU/g的大肠杆菌K99冻干粉溶解到10 mL生理盐水中对犊牛进行口服大肠杆菌攻毒,攻毒剂量参考Pal等[37]和Still等[38]。
犊牛出生后立即转移至1.5 m×3.0 m犊牛岛内实行单圈饲养,转移完成后立即借助食管导管饲喂4 L第1次挤的初乳,并在出生后6 h饲喂2 L第1次挤的初乳。每日分别在08:00和15:00饲喂常乳,饲喂量:第2~7天,2.5 L/次;第8~14天,4.5 L/次。自由饮水,开食料(乳倍优8100,内蒙古牧泉元兴饲料有限责任公司)从犊牛3日龄开始自由采食,不提供粗饲料。犊牛开食料主要原料包括压片玉米、豆粕、石粉、氯化钠、维生素A、维生素D3、DL-α-生育酚乙酸酯、硫酸铜、硫酸锰和硫酸锌等。初乳、常乳的密度及营养水平见表 1,开食料的营养水平见表 2。
|
|
表 1 初乳、常乳的密度及营养水平 Table 1 Density and nutrient levels of colostrum and milk |
|
|
表 2 开食料的营养水平(干物质基础) Table 2 Nutrient levels of starter (DM basis) |
在犊牛出生当日,收集每头犊牛饲喂的初乳,并每周采集犊牛饮用常乳和开食料样品,于-20 ℃保存。初乳和常乳营养成分使用乳成分分析仪(MilkoScan Type 78110,Foss Electric,丹麦)进行测定。参考AOAC(2000)[40]的方法测定开食料中DM、CP、粗脂肪(EE)和粗灰分(Ash)含量,参考Van Soest等[41]的方法测定开食料中酸性洗涤纤维(ADF)和中性洗涤纤维(NDF)含量,使用电感耦合等离子体发射光谱仪(ICP-OES,9000,Shimadzu,日本)测定开食料中钙(Ca)和磷(P)含量。其中,CP含量采用K1100全自动凯氏定氮仪测定,ADF和NDF含量采用Y078自动纤维测定仪(A2000i)测定,EE含量采用SoxtecTM 2050全自动脂肪分析仪测定。
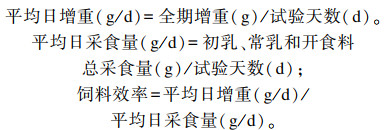
1.3.2 生长性能在犊牛出生当日及7、11和14日龄,晨饲前称重,并计算每头牛平均日增重(ADG)。记录每日常乳和开食料摄入量,计算每头牛平均日采食量(ADFI)和饲料效率。
|
于哺乳犊牛2日龄开始,每日07:00观察试验犊牛的粪便情况,并记录。采用表 3中的4分制粪便评分标准[42]进行评分,以粪便评分≥3为腹泻。
|
|
表 3 粪便评分标准 Table 3 Fecal score standard |
在犊牛7、11和14日龄午饲后2~3 h,颈静脉采血20 mL,血样于4 ℃、3 000×g离心20 min后,收集血清分装于5个2 mL离心管中,于-20 ℃保存。采用水溶性四氮唑-1(WST-1)法测定血清超氧化物歧化酶(SOD)活性,采用硫代巴比妥酸法测定血清丙二醛(MDA)含量,采用比色法测定血清谷胱甘肽过氧化物酶(GSH-Px)活性,采用钼酸铵法测定血清过氧化氢酶(CAT)活性,所采用的测定仪器为Y040多功能酶标仪(Tecan Infinite 200 Pro,Tecan国际有限公司)。上述指标测定所用试剂盒均购于南京建成生物工程研究所,具体操作方法参考试剂盒说明书。
1.4 数据统计分析数据分析应用SAS 9.4统计分析软件中关于重复测量数据的MIXED模型进行分析。差异显著时采用最小显著差数法(least significant difference,LSD)进行比较,P < 0.05为差异显著,0.05≤P < 0.10为有提高或降低的趋势。
2 结果 2.1 裂壶藻和乳铁蛋白对哺乳犊牛生长性能和粪便评分的影响由表 4可知,饲粮中添加裂壶藻和乳铁蛋白对大肠杆菌攻毒前(1~7日龄)、攻毒后(8~14日龄)犊牛平均日采食量和饲料效率无显著影响(P>0.05)。1~7日龄时,饲粮中添加裂壶藻有提高平均日增重的趋势(P=0.093)。8~11日龄时,与C组相比,LF、SZ和LF+SZ组犊牛粪便评分显著降低(P < 0.05),且乳铁蛋白和裂壶藻在降低粪便评分方面存在协同作用的趋势(P=0.074)。
|
|
表 4 裂壶藻和乳铁蛋白对哺乳犊牛生长性能和粪便评分的影响 Table 4 Effects of Schizochytrium sp. and lactoferrin on growth performance and fecal score of sucking calves |
由表 5可知,7日龄时,饲粮中添加乳铁蛋白和裂壶藻有提高犊牛血清CAT活性的趋势(P=0.055、P=0.091);11日龄时,与C组相比,LF、SZ和LF+SZ组犊牛血清CAT活性显著提高(P < 0.05),且LF+SZ组显著高于LF、SZ组(P < 0.05);14日龄时,LF+SZ组犊牛血清CAT活性显著高于SZ和C组(P < 0.05)。14日龄时,与C组相比,SZ和LF+SZ组犊牛血清SOD活性显著提高(P < 0.05),且乳铁蛋白和裂壶藻在提高犊牛血清SOD活性方面存在协同作用的趋势(P=0.063)。7日龄时,与SZ和LF+SZ组相比,LF组犊牛血清GSH-Px活性显著提高(P < 0.05)。7日龄时,饲粮中添加裂壶藻有提高血清MDA含量的趋势(P=0.055);11日龄时,与LF组相比,SZ和LF+SZ组犊牛血清MDA含量显著提高(P < 0.05),但与C组差异不显著(P>0.05);14日龄时,LF+SZ组犊牛血清MDA含量显著高于其他各组(P < 0.05)。
|
|
表 5 裂壶藻和乳铁蛋白对哺乳犊牛血清抗氧化指标的影响 Table 5 Effects of Schizochytrium sp. and lactoferrin on serum antioxidant indices of sucking calves |
大肠杆菌K99是引起新生犊牛腹泻的主要病原菌之一[43-44]。本试验对犊牛进行大肠杆菌攻毒处理后,研究了在攻毒条件下裂壶藻和乳铁蛋白对犊牛腹泻的缓解作用。结果显示,饲粮中添加乳铁蛋白对犊牛平均日增重、平均日采食量和饲料效率均无显著影响,而饲粮中添加裂壶藻有增加攻毒前犊牛平均日增重的趋势。研究发现,微藻中DHA可通过增加肌肉胰岛素样生长因子-1(IGF-1)的基因表达量,并激活胰岛素受体来增加肌肉蛋白质的合成,从而提高生长猪的生长性能[45],且有研究报道,n-3 PUFAs可改善动物机体肠道中的葡萄糖的吸收,增加了肌糖原的含量[46-47],进而裂壶藻通过影响机体蛋白质和能量代谢促进其平均日增重。Joslin等[33]研究发现,饲粮中添加0、1和10 g/d乳铁蛋白对1~2周龄犊牛体重没有显著影响,但可显著提高2周龄以后犊牛体重,这与本试验中乳铁蛋白并未提高犊牛生长性能的试验结果一致,这可能是由于常乳中提供了足够的乳铁蛋白。
肠道内大肠杆菌大量繁殖可导致肠道菌群失调并产生毒素,继而使小肠中水分和电解质含量发生改变,如果大肠不能将来自小肠的过多水分吸收则导致腹泻[48]。本试验中利用致病性大肠杆菌K99进行攻毒处理后,大部分犊牛出现了粪便评分升高的现象。同样,参考Pal等[37]和Still等[38]用致病性大肠杆菌O101:K99对犊牛攻毒后,也出现腹泻率增加的现象,这说明利用致病性大肠杆菌对犊牛进行攻毒是有效的。C组犊牛在攻毒后腹泻率为70%(7头牛发生腹泻,n=10),攻毒前腹泻率为30%(3头牛发生腹泻,n=10),且攻毒前3 d C组未发生犊牛腹泻。
本试验中,饲粮中添加裂壶藻和乳铁蛋白降低了犊牛的粪便评分。乳铁蛋白中带正电的氨基酸基团可以与某些病原微生物表面的阴离子基团结合,使细菌裂解,从而具有杀菌作用[49]。裂壶藻中的n-3 PUFAs可以改变细胞内的肠脂肪酸结合蛋白,激活过氧化物酶体增殖物,激活受体通路,上调紧密连接蛋白,提高抗性和减少白细胞介素介导的渗透性,从而可以保护肠道屏障完整性[50]。裂壶藻和乳铁蛋白通过上述2个方面的功效,促进犊牛肠道健康,有效降低犊牛腹泻。这可能是本试验中在对犊牛进行大肠杆菌攻毒之前添加裂壶藻和乳铁蛋白可以有效缓解犊牛腹泻的潜在原因。
3.2 裂壶藻和乳铁蛋白对哺乳犊牛血清抗氧化指标的影响胃肠道是一个复杂的动态平衡系统,由上皮屏障、免疫介质和微生物群落组成[51]。新生婴幼儿和新生幼龄动物在胃肠道内没有建立适当的动态平衡时,会出现氧化应激[51-52]。有研究发现,氧化应激可能是机体营养不良时引起肠功能障碍的主要原因[53-54],且活性氧(reactive oxygen species,ROS)在发生慢性腹泻时会导致电解质的丢失和黏膜通透性的增加[55]。氧化应激可改变机体抗氧化防御能力,增加肠道内水分的分泌,从而引起腹泻[56-57]。营养不良会增加肠道固有层内淋巴细胞的浸润,从而产生氧化应激损伤[58]。断奶腹泻与肠道黏膜氧化应激之间存在密切相关关系[59],且肠道黏膜氧化应激可引起机体腹泻[52, 60-61]。本试验中,哺乳犊牛处于腹泻应激状态,进而可打破机体抗氧化与促氧化之前的平衡,改变抗氧化的发生,出现氧化胁迫,产生过多的自由基。当机体不能及时有效地去除自由基时,可损伤动物机体健康。
SOD和GSH-Px是降低氧化应激的主要抗氧化酶[62]。脂质过氧化程度常被用作ROS介导的损伤指标[63],SOD可以催化超氧化物转变为过氧化氢(H2O2),被认为是抗氧化的第1道防线[64-65],而CAT能特异性清除体内过多的H2O2,保护细胞免受过氧化损伤。本试验中,饲粮中添加乳铁蛋白、裂壶藻和乳铁蛋白+裂壶藻可提高犊牛血清CAT活性,且饲粮中添加裂壶藻和乳铁蛋白+裂壶藻可提高犊牛血清SOD活性。其作用机制可能是由于裂壶藻中的n-3 PUFAs通过线粒体呼吸链反应促进超氧阴离子(O2-)的形成,进而提高SOD的活性,又因SOD可催化超氧阴离子形成H2O2,而H2O2可在CAT的催化下形成水和氧气,进而清除机体内过多的H2O2[66]。
乳铁蛋白与裂壶藻相比,可提高血清GSH-Px活性,其机制可能是由于乳铁蛋白能结合三价铁离子(Fe3+),减少氧自由基反应(Haber-Weiss反应)的生成,抑制Fe3+参与的脂质氧化,使机体避免受到金属离子的诱导氧化,同时在肠道吸收过程中,乳铁蛋白与微量元素结合,使血液中铜、锌和硒等微量元素含量升高,而作为GSH-Px重要的辅酶、辅基或酶激活剂,这些微量元素可以显著提高GSH-Px活性[26]。谷胱甘肽(glutathione,GSH)和GSH-Px已被证明对于保护胃肠道黏膜细胞免受放射线、内毒素和ROS等的损伤有重要作用[67],进而乳铁蛋白通过提高GSH-Px的活性,保护机体免受大肠杆菌分泌的内毒素的损伤,并有效降低犊牛腹泻。
血液和组织中MDA通常被用作自由基诱导损伤和内源性脂质过氧化的生物标志物[68-70],可以反映机体受到自由基攻击的程度。本试验中,与乳铁蛋白相比,饲粮中添加裂壶藻可提高血清MDA含量,这与Mavrommatis等[71]对山羊的研究结果一致,其结果显示随着裂壶藻添加水平的增加,血浆MDA含量增加,这可能与裂壶藻富含n-3 PUFAs有关。有研究发现,n-3 PUFAs的来源及其在饲粮中的含量都会影响动物机体目标组织的氧化状态[72-74],且乳铁蛋白能够抑制铁诱导过氧化反应过程中产生的MDA、硫代巴比妥酸,进而阻断生成氧自由基的途径[75]。但饲粮中同时添加乳铁蛋白和裂壶藻组并未能降低犊牛血清中MDA含量,这可能是由于乳铁蛋白不足以缓解由饲粮中n-3 PUFA增加而导致的过氧化物增加。饲粮中添加裂壶藻和乳铁蛋白均可提高机体抗氧化能力,但乳铁蛋白的抗氧化能力优于裂壶藻。
4 结论犊牛在大肠杆菌K99攻毒条件下,饲粮中添加裂壶藻和乳铁蛋白具有促进肠道健康、降低腹泻、提高抗氧化能力的作用。乳铁蛋白提高犊牛抗氧化能力方面优于裂壶藻,且裂壶藻和乳铁蛋白联合使用在降低哺乳犊牛粪便评分方面有协同作用,可更好地缓解犊牛腹泻。
| [1] |
HEINRICHS A J, HEINRICHS B S. A prospective study of calf factors affecting first-lactation and lifetime milk production and age of cows when removed from the herd[J]. Journal of Dairy Science, 2011, 94(1): 336-341. DOI:10.3168/jds.2010-3170 |
| [2] |
SOBERON F, RAFFRENATO E, EVERETT R W, et al. Preweaning milk replacer intake and effects on long-term productivity of dairy calves[J]. Journal of Dairy Science, 2012, 95(2): 783-793. DOI:10.3168/jds.2011-4391 |
| [3] |
BUTLER D G, CLARKE R C.Diarrhoea and dysentery in calves[M]//GYLES C L.Escherichia coli in domestic animals and humans.Wallingford: CAB International, 1994: 91-116.
|
| [4] |
IZZO M M, KIRKLAND P D, MOHLER V L, et al. Prevalence of major enteric pathogens in Australian dairy calves with diarrhoea[J]. Australian Veterinary Journal, 2011, 89(5): 167-173. DOI:10.1111/j.1751-0813.2011.00692.x |
| [5] |
CHO Y I, YOON K J. An overview of calf diarrhea-infectious etiology, diagnosis, and intervention[J]. Journal of Veterinary Science, 2014, 15(1): 1-17. DOI:10.4142/jvs.2014.15.1.1 |
| [6] |
YIMER M, GEZHAGNE M, BIRUK T, et al. A review on major bacterial causes of calf diarrhea and its diagnostic method[J]. Journal of Veterinary Medicine and Animal Health, 2015, 7(5): 173-185. DOI:10.5897/JVMAH2014.0351 |
| [7] |
TRIPATHI N N, MISHRA A K, TRIPATHI S. Antibacterial potential of plant volatile oils:a review[J]. Proceedings of the National Academy of Sciences, India-Section B:Biological Sciences, 2011, 81: 23-68. |
| [8] |
MOSELE J I, MACIA A, MOTILVA M J. Metabolic and microbial modulation of the large intestine ecosystem by non-absorbed diet phenolic compounds:a review[J]. Molecules, 2015, 20(9): 17429-17468. DOI:10.3390/molecules200917429 |
| [9] |
BRENES A, VIVEROS A, CHAMORRO S, et al. Use of polyphenol-rich grape by-products in monogastric nutrition.A review[J]. Animal Feed Science and Technology, 2016, 211: 1-17. DOI:10.1016/j.anifeedsci.2015.09.016 |
| [10] |
FLAGA J, KORYTKOWSKI Ł, GÓRKA P, et al. The effect of docosahexaenoic acid-rich algae supplementation in milk replacer on performance and selected immune system functions in calves[J]. Journal of Dairy Science, 2019, 102(10): 8862-8873. DOI:10.3168/jds.2018-16189 |
| [11] |
CHOI Y, GOEL A, HOSSEINDOUST A, et al. Effects of dietary supplementation of Ecklonia cava with or without probiotics on the growth performance, nutrient digestibility, immunity and intestinal health in weanling pigs[J]. Italian Journal of Animal Science, 2016, 15(1): 62-68. DOI:10.1080/1828051X.2015.1128685 |
| [12] |
GEBERT S, DAVIS E, REHBERGER T, et al. Lactobacillus brevis strain 1E1 administered to piglets through milk supplementation prior to weaning maintains intestinal integrity after the weaning event[J]. Beneficial Microbes, 2011, 2(1): 35-45. DOI:10.3920/BM2010.0043 |
| [13] |
YU J H, WANG Y, SUN J, et al. Antioxidant activity of alcohol aqueous extracts of Crypthecodinium cohnii and Schizochytrium sp.[J]. Journal of Zhejiang University-Science B, 2017, 18(9): 797-806. DOI:10.1631/jzus.B1600367 |
| [14] |
SIJBEN J W, CALDER P C. Differential immunomodulation with long-chain n-3 PUFA in health and chronic disease[J]. Proceedings of the Nutrition Society, 2007, 66(2): 237-259. DOI:10.1017/S0029665107005472 |
| [15] |
CALDER P C, GRIMBLE R F. Polyunsaturated fatty acids, inflammation and immunity[J]. European Journal of Clinical Nutrition, 2002, 56(Suppl.3): 14-19. |
| [16] |
KEW S, MESA M D, TRICON S T, et al. Effects of oils rich in eicosapentaenoic and docosahexaenoic acids on immune cell composition and function in healthy humans[J]. The American Journal of Clinical Nutrition, 2004, 79(4): 674-681. DOI:10.1093/ajcn/79.4.674 |
| [17] |
JHO D H, COLE S M, LEE E M, et al. Role of omega-3 fatty acid supplementation in inflammation and malignancy[J]. Integrative Cancer Therapies, 2004, 3(2): 98-111. DOI:10.1177/1534735404264736 |
| [18] |
SHIMAZAWA M, NAKAJIMA Y, MASHIMA Y, et al. Docosahexaenoic acid (DHA) has neuroprotective effects against oxidative stress in retinal ganglion cells[J]. Brain Research, 2009, 1251: 269-275. DOI:10.1016/j.brainres.2008.11.031 |
| [19] |
TSIPLAKOU E, CHATZIKONSTANTINOU M, MITSIOPOULOU C, et al. Effect of soya bean and fish oil inclusion in diets on milk and plasma enzymes from sheep and goat related to oxidation[J]. Journal of Animal Physiology and Animal Nutrition, 2017, 101(4): 733-742. DOI:10.1111/jpn.12516 |
| [20] |
LI M H, ROBINSON E H, TUCKER C S, et al. Effects of dried algae Schizochytrium sp., a rich source of docosahexaenoic acid, on growth, fatty acid composition, and sensory quality of channel catfish Ictalurus punctatus[J]. Aquaculture, 2009, 292(3-4): 232-236. DOI:10.1016/j.aquaculture.2009.04.033 |
| [21] |
SIMOPOULOS A P, LEAF A, SALEM N S Jr. Workshop on the essentiality of and recommended dietary intakes for omega-6 and omega-3 fatty acids[J]. Asia Pacific Journal of Clinical Nutrition, 1999, 8(4): 300-301. DOI:10.1046/j.1440-6047.1999.00123.x |
| [22] |
MEADUS W J, DUFF P, ROLLAND D, et al. Feeding docosahexaenoic acid to pigs reduces blood triglycerides and induces gene expression for fat oxidation[J]. Canadian Journal of Animal Science, 2011, 91(4): 601-612. DOI:10.4141/cjas2011-055 |
| [23] |
SHIN K, YAMAUCHI K, TERAGUCHI S, et al. Antibacterial activity of bovine lactoferrin and its peptides against enterohaemorrhagic Escherichia coli O157:H7[J]. Letters in Applied Microbiology, 1998, 26(6): 407-411. DOI:10.1046/j.1472-765X.1998.00358.x |
| [24] |
TOMITA M, BELLAMY W, TAKASE M, et al. Potent antibacterial peptides generated by pepsin digestion of bovine lactoferrin[J]. Journal of Dairy Science, 1991, 74(12): 4137-4142. DOI:10.3168/jds.S0022-0302(91)78608-6 |
| [25] |
REITER B, BROCK J H, STEEL E D. Inhibition of Escherichia coli by bovine colostrum and post colostral milk.Ⅱ.The bacteriostatic effect of lactoferrin on a serum susceptible and serum resistant strain of E.coli[J]. Immunology, 1975, 28(1): 83-95. |
| [26] |
KUME S I, TANABE S. Effect of supplemental lactoferrin with ferrous iron on iron status of newborn calves[J]. Journal of Dairy Science, 1996, 79(3): 0-464. |
| [27] |
MIYAUCHI H, HASHIMOTO S I, NAKAJIMA M, et al. Bovine lactoferrin stimulates the phagocytic activity of human neutrophils:identification of its active domain[J]. Cellular Immunology, 1998, 187(1): 34-37. DOI:10.1006/cimm.1997.1246 |
| [28] |
EMBLETON N D, BERRINGTON J E, MCGUIRE W, et al. Lactoferrin:antimicrobial activity and therapeutic potential[J]. Seminars in Fetal and Neonatal Medicine, 2013, 18(3): 143-149. DOI:10.1016/j.siny.2013.02.001 |
| [29] |
HIROTANI Y, IKEDA K, KATO R, et al. Protective effects of lactoferrin against intestinal mucosal damage induced by lipopolysaccharide in human intestinal Caco-2 cells[J]. Yakugaku Zasshi, 2008, 128(9): 1363-1368. DOI:10.1248/yakushi.128.1363 |
| [30] |
TERAGUCHI S, OZAWA K, YASUDA S, et al. The bacteriostatic effects of orally administered bovine lactoferrin on intestinal Enterobacteriaceae of SPF mice fed bovine milk[J]. Bioscience, Biotechnology, and Biochemistry, 1994, 58(3): 482-487. DOI:10.1271/bbb.58.482 |
| [31] |
ZHANG P, SAWICKI B, HANSON L, et al. Human lactoferrin in the milk of transgenic mice increases intestinal growth in ten-day-old suckling neonates[J]. Advances in Experimental Medicine and Biology, 2001, 501: 107-113. |
| [32] |
OGATA T, TERAGUCHI S, SHIN K, et al.The mechanism of in vivo bacteriostasis of bovine lactoferrin[M]//SPIK G, LEGRAND D, MAZURIER J, et al.Advances in lactoferrin research.Boston: Springer, 1998, 443: 239-246.
|
| [33] |
JOSLIN R S, ERICKSON P S, SANTORO H M, et al. Lactoferrin supplementation to dairy calves[J]. Journal of Dairy Science, 2002, 85(5): 1237-1242. DOI:10.3168/jds.S0022-0302(02)74187-8 |
| [34] |
ROBBLEE E D, ERICKSON P S, WHITEHOUSE N L, et al. Supplemental lactoferrin improves health and growth of Holstein calves during the preweaning phase[J]. Journal of Dairy Science, 2003, 86(4): 1458-1464. DOI:10.3168/jds.S0022-0302(03)73729-1 |
| [35] |
YEKTA M A, COX E, GODDEERIS B M, et al. Reduction of Escherichia coli O157:H7 excretion in sheep by oral lactoferrin administration[J]. Veterinary Microbiology, 2011, 150(3/4): 373-378. |
| [36] |
KIECKENS E, RYBARCZYK J, DE ZUTTER L, et al. Clearance of Escherichia coli O157:H7 infection in calves by rectal administration of bovine lactoferrin[J]. Applied and Environmental Microbiology, 2015, 81(5): 1644-1651. DOI:10.1128/AEM.03724-14 |
| [37] |
PAL B, PACHAURI S P. Effect of oral rehydration in neonatal calves treated for diarrhoea induced with Escherichia coli (0101:K99) infection[J]. The Indian Journal of Veterinary Research, 2008, 17(1): 19-26. |
| [38] |
STILL J, DELAHAUT P, COPPE P, et al. Treatment of induced enterotoxigenic colibacillosis (Scours) in calves by the lactoperoxidase system and lactoferrin[J]. Annals of Veterinary Research, 1990, 21(2): 143-152. |
| [39] |
NRC.Nutrient requirements of dairy cattle[S].7th ed.Washington, D.C.National Academy of Science, 2001.
|
| [40] |
AOAC.Official methods of analysis of the association of official analytical chemists[S].17th ed.Washington D.C.: AOAC, 2000.
|
| [41] |
VAN SOEST P J, ROBERTSON J B, LEWIS B A. Symposium:carbohydrate methodology, metabolism, and nutritional implications in dairy cattle[J]. Journal of Dairy Science, 1991, 74(10): 3583-3597. DOI:10.3168/jds.S0022-0302(91)78551-2 |
| [42] |
MAGALHÃES V J, SUSCA F, LIMA F S, et al. Effect of feeding yeast culture on performance, health, and immunocompetence of dairy calves[J]. Journal of Dairy Science, 2008, 91(4): 1497-1509. DOI:10.3168/jds.2007-0582 |
| [43] |
SHAMS Z, TAHAMTAN Y, POURBAKHSH A, et al. Detection of enterotoxigenic K99(F5) and F41 from fecal sample of calves by molecular and serological methods[J]. Comparative Clinical Pathology, 2012, 21(4): 475-478. DOI:10.1007/s00580-010-1122-2 |
| [44] |
OK M, GVLER L, TURGUT K, et al. The studies on the aetiology of diarrhoea in neonatal calves and determination of virulence gene markers of Escherichia coli strains by multiplex PCR[J]. Zoonoses and Public Health, 2010, 56(2): 94-101. |
| [45] |
WEI H K, ZHOU Y F, JIANG S Z, et al. Feeding a DHA-enriched diet increases skeletal muscle protein synthesis in growing pigs:association with increased skeletal muscle insulin action and local mRNA expression of insulin-like growth factor[J]. British Journal of Nutrition, 2013, 110(4): 671-680. DOI:10.1017/S0007114512005740 |
| [46] |
LEONARD S G, SWEENEY T, BAHAR B, et al. Effect of dietary seaweed extracts and fish oil supplementation in sows on performance, intestinal microflora, intestinal morphology, volatile fatty acid concentrations and immune status of weaned pigs[J]. British Journal of Nutrition, 2011, 105(4): 549-560. DOI:10.1017/S0007114510003739 |
| [47] |
GABLER N K, SPENCER J D, WEBEL D M, et al. In utero and postnatal exposure to long chain (n-3) PUFA enhances intestinal glucose absorption and energy stores in weanling pigs[J]. The Journal of Nutrition, 2007, 137(11): 2351-2358. DOI:10.1093/jn/137.11.2351 |
| [48] |
MOON H W, ISAACSON R E, POHLENZ J. Mechanisms of association of enteropathogenic Escherichia coli with intestinal epithelium[J]. The American Journal of Clinical Nutrition, 1979, 32(1): 119-127. DOI:10.1093/ajcn/32.1.119 |
| [49] |
ELASS-ROCHARD E, ROSEANU A, LEGRAND D, et al. Lactoferrin-lipopolysaccharide interaction:involvement of the 28-34 loop region of human lactoferrin in the high-affinity binding to Escherichia coli 055B5 lipopolysaccharide[J]. Biochemical Journal, 1995, 312(3): 839-845. DOI:10.1042/bj3120839 |
| [50] |
WANG X Y, PAN L Y, LU J, et al. n-3 PUFAs attenuate ischemia/reperfusion induced intestinal barrier injury by activating Ⅰ-FABP-PPARγ pathway[J]. Clinical Nutrition, 2012, 31(6): 951-957. DOI:10.1016/j.clnu.2012.03.003 |
| [51] |
MCCRACKEN V J, LORENZ R G. The gastrointestinal ecosystem:a precarious alliance among epithelium, immunity and microbiota[J]. Cellular Microbiology, 2001, 3: 1-11. DOI:10.1046/j.1462-5822.2001.00090.x |
| [52] |
KHALED M A. Oxidative stress in childhood malnutrition and diarrhoeal diseases[J]. Journal of Diarrhoeal Diseases Research, 1994, 12(3): 165-172. |
| [53] |
GOLDEN M H, RAMDATH D D. Free radicals in the pathogenesis of kwashiorkor[J]. Proceedings of the Nutrition Society, 1987, 46(1): 53-68. DOI:10.1079/PNS19870008 |
| [54] |
GODIN D V, WOHAIEB S A. Nutritional deficiency, starvation, and tissue antioxidant status[J]. Free Radical Biology and Medicine, 1988, 5(3): 165-176. DOI:10.1016/0891-5849(88)90079-2 |
| [55] |
KONINGSBERGER J C, MARX J J, VAN HATTUM C. Radicals in gastroenterology[J]. Scandinavian Journal of Gastroenterology, 1965, 23(4): 30-40. |
| [56] |
DARMON N, PÉLISSIER M G, HEYMAN M, et al. Oxidative stress may contribute to the intestinal dysfunction of weanling rats fed a low protein diet[J]. Journal of Nutrition, 1993, 123(6): 1068-1075. |
| [57] |
LINDLEY K J, GOSS-SAMPSON M A, MULLER D P R, et al. Lipid peroxidation and electrogenic ion transport in the jejunum of the vitamin E deficient rat[J]. Gut, 1994, 35(1): 34-39. DOI:10.1136/gut.35.1.34 |
| [58] |
HUANG C J, FWU M L. Protein insufficiency aggravates the enhanced lipid peroxidation and reduced activities of antioxidative enzymes in rats fed diets high in polyunsaturated fat[J]. The Journal of Nutrition, 1990, 122(5): 1182-1189. |
| [59] |
SONG P X, ZHANG R J, WANG X X, et al. Dietary grape-seed procyanidins decreased postweaning diarrhea by modulating intestinal permeability and suppressing oxidative stress in rats[J]. Journal of Agricultural and Food Chemistry, 2011, 59(11): 6227-6232. DOI:10.1021/jf200120y |
| [60] |
WANG X Q, OU D Y, YIN J D, et al. Proteomic analysis reveals altered expression of proteins related to glutathione metabolism and apoptosis in the small intestine of zinc oxide-supplemented piglets[J]. Amino Acids, 2009, 37(1): 209-218. DOI:10.1007/s00726-009-0242-y |
| [61] |
DI PAOLA R, ESPOSITO E, MAZZON E, et al. 3, 5-dicaffeoyl-4-malonylquinic acid reduced oxidative stress and inflammation in a experimental model of inflammatory bowel disease[J]. Free Radical Research, 2010, 44(1): 74-89. |
| [62] |
LANGIE S A S, WILMS L C, HÄMÄLÄINEN S, et al. Modulation of nucleotide excision repair in human lymphocytes by genetic and dietary factors[J]. The British Journal of Nutrition, 2010, 103(4): 490-501. DOI:10.1017/S0007114509992066 |
| [63] |
KVHN H, BORCHERT A. Regulation of enzymatic lipid peroxidation:the interplay of peroxidizing and peroxide reducing enzymes[J]. Free Radical Biology and Medicine, 2002, 33(2): 154-172. DOI:10.1016/S0891-5849(02)00855-9 |
| [64] |
HALLIWELL B, CHIRICO S. Lipid peroxidation:its mechanism, measurement, and significance[J]. American Journal of Clinical Nutrition, 1993, 57(Suppl.1): 715S-725S. |
| [65] |
DAS K, ROYCHOUDHURY A. Reactive oxygen species (ROS) and response of antioxidants as ROS-scavengers during environmental stress in plants[J]. Frontiers in Environmental Science, 2014, 2: 53. |
| [66] |
LYKKESFELDT J, SVENDSEN O. Oxidants and antioxidants in disease:oxidative stress in farm animals[J]. The Veterinary Journal, 2007, 173(3): 502-511. DOI:10.1016/j.tvjl.2006.06.005 |
| [67] |
WU G Y, FANG Y Z, YANG S, et al. Glutathione metabolism and its implications for health[J]. The Journal of Nutrition, 2004, 134(3): 489-492. DOI:10.1093/jn/134.3.489 |
| [68] |
YOUSEF M I, SAAD A A, EL-SHENNAWY L K. Protective effect of grape seed proanthocyanidin extract against oxidative stress induced by cisplatin in rats[J]. Food and Chemical Toxicology, 2009, 47(6): 1176-1183. DOI:10.1016/j.fct.2009.02.007 |
| [69] |
NIELSEN F, MIKKELSEN B B, BO NIELSEN J, et al. Plasma malondialdehyde as biomarker for oxidative stress:reference interval and effects of life-style factors[J]. Clinical Chemistry, 1997, 43(7): 1209-1214. DOI:10.1093/clinchem/43.7.1209 |
| [70] |
GROTTO D, MARIA L S, VALENTINI J, et al. Importance of the lipid peroxidation biomarkers and methodological aspects FOR malondialdehyde quantification[J]. Química Nova, 2009, 32(1): 169-174. DOI:10.1590/S0100-40422009000100032 |
| [71] |
MAVROMMATIS A, CHRONOPOULOU E G, SOTIRAKOGLOU K, et al. The impact of the dietary supplementation level with Schizochytrium sp, on the oxidative capacity of both goats' organism and milk[J]. Livestock Science, 2018, 218: 37-43. DOI:10.1016/j.livsci.2018.10.014 |
| [72] |
RUIZ-GUTIÉRREZ V, PÉREZ-ESPINOSA A, VÁZQUEZ C M, et al. Effects of dietary fats (fish, olive and high-oleic-acid sunflower oils) on lipid composition and antioxidant enzymes in rat liver[J]. British Journal of Nutrition, 1999, 82(3): 233-241. DOI:10.1017/S0007114599001415 |
| [73] |
YUAN Y V, KITTS D D. Dietary (n-3) fat and cholesterol alter tissue antioxidant enzymes and susceptibility to oxidation in SHR and WKY rats[J]. Jrounal of Nutrition, 2003, 133(3): 679-688. |
| [74] |
YUAN Y V, KITTS D D. Dietary fat source and cholesterol interactions alter plasma lipids and tissue susceptibility to oxidation in spontaneously hypertensive (SHR) and normotensive Wistar Kyoto (WKY) rats[J]. Molecular and Cellular Biochemistry, 2002, 232(1/2): 33-47. DOI:10.1023/A:1014837131439 |
| [75] |
LINDMARK-MÁNSSON H, AKESSON B. Antioxidative factors in milk[J]. British Journal of Nutrition, 2000, 84(Suppl.1): S103-S110. |




